New strategy to combat bacterial infections
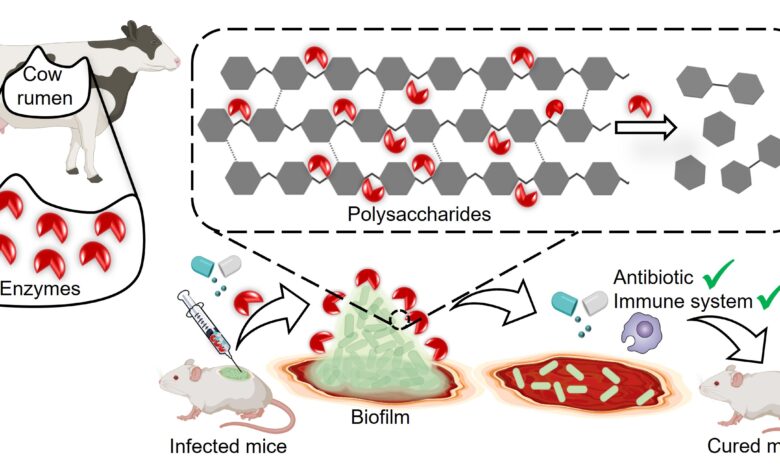
Most of the disease-causing bacteria secrete matrix-like layers around themselves called biofilms. These biofilms act as thick barriers limiting the entry of drugs and helping the bacteria become resistant to antibiotics.
Klebsiella pneumoniae is one of them. It is an opportunistic bacterium that infects patients in hospitals, causing conditions like pneumonia, urinary tract infections, and meningitis. In people with diabetes, it infects wounds which end up healing slowly, leading to complications that may sometimes result in amputation of a limb.
It secretes a tough biofilm made up mostly of sugars, fats, proteins, and DNA. Strings of sugar molecules come together to form polysaccharides, which play a key role in making the biofilm stronger.
In a new study, a team of researchers from Bengaluru-based Indian Institute of Science (IISc) explored the gut of the cow to figure out a solution as it harbours several microbial enzymes that digest different kinds of complex polysaccharides, such as cellulose and hemicellulose, which the animal takes in from its plant food. Cellulosic polysaccharides are very similar to the ones in the bacterial biofilms.
The team focused on a set of enzymes called glycoside hydrolases (GH), looking closely at their protein structures to identify the ones that could potentially break down polysaccharides efficiently. They narrowed down on one enzyme found in the rumen, the largest stomach compartment in the cow.
They named it GH-B2 and artificially synthesised it in the lab. When they tested the lab-made GH-B2 on four different strains of K. pneumoniae isolated from different hospital patients, they found that it successfully broke down biofilms in all four.
“Such broad activity of the enzyme was surprising, as the strains were different in terms of their serotypes,” said Debasis Das, Assistant Professor in the Department of Inorganic and Physical Chemistry (IPC) and corresponding author of the study.
The researchers found that treating a mature biofilm with the enzyme made the bacteria 15 times more susceptible to a broad-spectrum antibiotic called meropenem. When they added the enzyme at the start of biofilm formation, the enzyme prevented the biofilm from developing altogether, and the bacteria became 250 times more susceptible to the antibiotic. The biofilm breakdown also made K. pneumoniae more vulnerable to attack by immune cells from mice and humans.

The team also tested their enzyme in lab mice that had wounds infected by K. pneumoniae. Treating the wound with both the enzyme and meropenem caused the biofilms to clear up completely.
Reshma Ramakrishnan, PhD student in Das’s lab and first author of the study, noted that the chances of the bacteria gaining resistance to the enzyme are very less because the enzyme was just disrupting the matrix and is not harming the bacteria directly. It will be a combinatorial therapy: the enzyme plus the antibiotic for treating K. pneumoniae biofilm-associated infections.
A IISc press release said the researchers are now planning on incorporating the enzyme in something wearable, like a wound dressing. “[For] local infections, specifically skin infections in diabetic individuals, this can be very promising,” says Dipshikha Chakravortty, Professor at the Department of Microbiology and Cell Biology (MCB) and another corresponding author of the study. The research team has published a report on their study in the science journal, npj Biofilms and Microbes.